Scars: How They Develop, Scar Removal Treatments, and Heparin-Based Creams

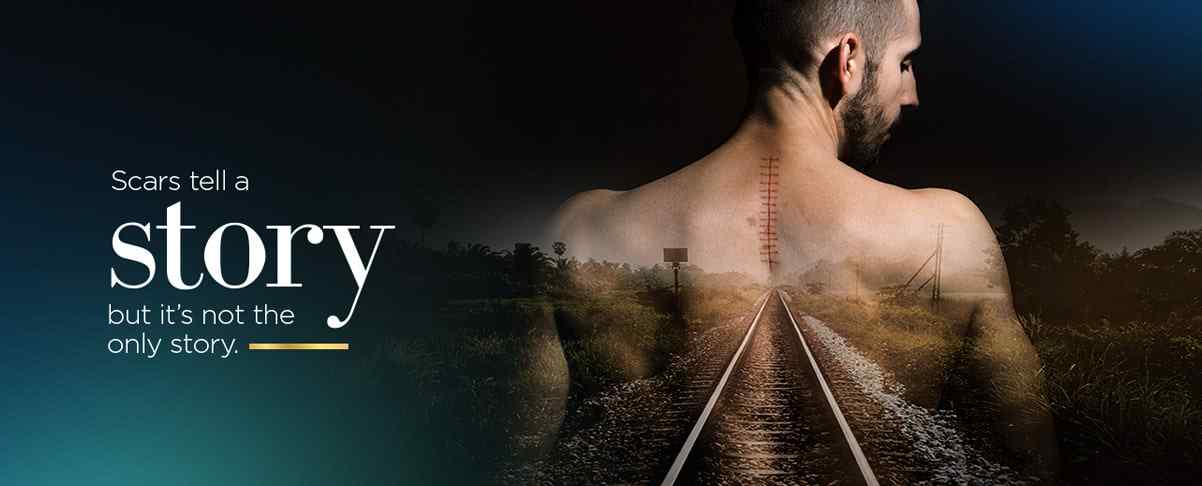
Sometimes, we wear our scars with pride—they signify something important to us or offer a sign of resilience, such as a hurdle we overcame. However, many scars are not a positive part of our body or our perceived body image. In fact, some scars can be all-out detrimental to self-confidence, our ability to interact openly with others, or even lead an ordinary life.
The majority of people have at least one scar somewhere on their bodies. About 100 million patients develop new scars with injuries or medical procedures on an annual basis. A prominent scar in the wrong place can have such a negative impact that it affects your own mental health substantially. People who have especially disfiguring or visible scars can face everything from anxiety and depression to diminished quality of life.
Over the years, a great deal of trial-and-error and legitimate research has been dedicated to diminishing scar tissue to enhance aesthetic appearance. While some efforts have not been in vain, many scar removal and minimizing practices have produced minimal results at best. Could a heparin-based cream for scars hold more promise? Here is a closer look at types of scars, how they form, and traditional and newfound scar treatment options.
Scars can stem from pretty much any type of skin injury, whether it is a burn, cut, puncture, or otherwise. Therefore, people develop scars after an array of different situations. Many scars are the basic result of some type of injury-causing event, such as being bitten by an animal, suffering a burn, or sustaining a cut during a car accident.
Scars can also emerge due to illness or skin issues, like a severe skin infection, acne, or even chickenpox. Many scars are the result of either necessary or elective surgeries. For instance, a mother ends up with a scar after a cesarean, a cosmetic surgery patient develops a face scar after a procedure, and an individual has a scar left behind after orthopedic surgery.
Regardless of what initially causes the scar, or even what type of scar you have, the formation of that scar tends to happen in the exact same process. When the skin sustains an injury, this important healing process takes place, which involves the activation of the skin's repair response. New skin cells are formed to close and protect the wound, but this natural healing process can sometimes be overly aggressive in nature. Let's take a closer look at the wound healing and scar development process.
Inflammation Phase
The inflammation phase is perhaps one of the most important after your skin has sustained some type of injury. Directly after the injury, the injured skin cells release inflammatory proteins called cytokines, which immediately triggers the immune system to send repair cells to get to work at the site of the injury by deterring bacteria and protecting the damaged tissue. More blood is delivered to the site to support the rapid processes that are taking place.
Proliferation Phase
With the injured area aptly protected, the number of fibroblast cells increases dramatically. Fibroblast cells deliver new collagen and other structural proteins, which play a key role in the wound-healing process. The structural proteins and collagen essentially build new skin tissue by creating a structural support network as quickly as possible to close the wound and protect the body.
Maturation Phase
The maturation phase is the final process in scar development and wound healing. Through a regulated process, some of the delivered proteins and collagen that created the structured support system for new skin start to break down because the new skin cells have matured. Think of this process as taking supports away from a concrete wall after the concrete has cured.
The end appearance of a scar can be affected either positively or negatively by the events that take place in any of these phases of wound healing. One of the most important phases is the inflammation phase, because the level of initial cytokines delivered to the area and how the immune system cells respond lay the groundwork for everything that happens beyond that point. For example, profound inflammation and cytokines may mean more collagen and structural protein deposits during the proliferation phases, so some of the structure of the scar may not fully degrade even once the maturation process has started.
All scars develop through the same basic processes within the body, but not all scars take on the same appearance. Scars can range in color, from red to brown to pale and skin-toned. They can be raised and smooth or broad and pitted or even sunken. Scars are often designated as a certain type based on their appearance or formation.
Keloid Scars
The keloid scar is a form of scar tissue that expands beyond the actual site of the wound, usually bulging upward and outward from the injury site. For example, an individual may develop a keloid scar after an ear-piercing that bulges outward on the back of their ear. Keloid scarring is thought to have a genetic component, and may not necessarily be related to the type of injury that caused the scar. An individual may see the same keloid formations whether they sustain a scratch or a puncture wound.
Hypertrophic Scars
Hypertrophic scars tend to be raised from the site of the skin wound and thick, but they usually stay within the boundaries of the wound site, unlike keloids. Oftentimes, the scar will be highly pigmented, possibly red or pink, and can even cause itching or burning sensations. These scars often go through a period of fading over time, but never fully go away.
Atrophic Scars
Atrophic scars are pitted or appear as an indention at the site of a prior wound. For example, someone who has undergone surgery that required a deep incision may have an atrophic scar. In these cases, the body simply could not generate enough new tissue to completely fill the opened area. However, atrophic scars are not always large; people who have experienced acne often develop pitted face scars.
A great deal of scar removal and minimizing treatments have been tried over the years. Some methods offer some change in the prominence of a scar, but not every treatment offers results for each individual. In general, scar treatments can be categorized by non-invasive and invasive treatments.
Non-Invasive
Non-invasive scar treatments are things like steroidal injections, silicone gel to reduce burn scars, chemical peels, or scar cream to simply lighten the appearance or soothe the formation of a scar. In some cases, interrupting the wound healing process with specific treatments may also be used. For instance, compression may be used on a prominent wound to deter the formation of a hypertrophic scar.
Invasive
Invasive treatment for scars tends to involve some form of surgery or scar tissue removal. For example, a keloid may be surgically removed or an atrophic scar may be cosmetically treated through skin grafts or other methodologies. While some more invasive treatments can be effective, some can also be related to further scarring, specifically for patients prone to keloid scars.
One of the most promising ways to treat several types of scars in a non-invasive way involves the use of topically applied scar cream. Scar creams are formulated with a number of beneficial agents that may target the specific issues that are making a scar either uncomfortable or highly visible. Heparin-based scar cream is an excellent example.
Heparin is an anticoagulant agent often used to prevent the formation of blood clots, but the agent has been proven to be medically useful for a range of other issues as well. While the mechanisms of how heparin may help with scarring are not completely understood, medical professionals speculate that the agent may reduce inflammation, irritation, and microbes in the area of a wound or scar.
A heparin-based cream called Contractubex has actually been in use for decades in several countries. In Contractubex gel, heparin is combined with other supportive agents like allantoin and extractum cepae. In the published studies on scar removal or minimization with heparin-based creams, the outcomes have proven to be quite remarkable.
In a study of young thoracic surgery patients, 90 percent of patients experienced either good or very good scar development. Additionally, fewer patients developed either keloid scars or hypertrophic scars. Contractubex was also shown to be significantly more effective at improving redness, discomfort, and consistency of scars compared to steroid treatment. Perhaps most notable, a study of 61 women with significant scarring after a c-section was evaluated after being given either heparin-based scar cream or a placebo. Researchers found the treatment group had more than a 14 percent improvement in the appearance of their scars. The scars were assessed for color, rigidity, and irregularity.
At Harbor Compounding Pharmacy, we understand that some scars can impede your ability to live your best life. The idea that something like a scar can cause such painful consequences spurred our team to do extensive research into the best scar cream options, pharmaceutical agents that have proven to be beneficial, and more.
If you have a scar that you would prefer to make a less prominent part of your appearance and your life, please reach out to us to discuss your options. Our compounding pharmacists can create a customized scar cream most suited to offer results with the type of scar you have. Give us a call today to find out how we can help.